Grand Rapids, MI – The Grand Rapids African American Health Institute (GRAAHI) is proud to announce its strong support and active participation in a critical campaign launched by the Advocacy Action Team for the Kent County Health Equity Council. We are rallying together with a sense of urgency to protect Medicaid from devastating proposed cuts that could impact hundreds of thousands of Michiganders. The bill threatening these vital healthcare services is scheduled for a vote as early as May 29th.
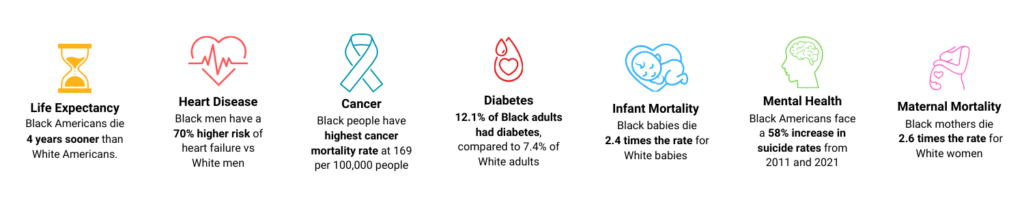
This isn’t just about numbers on a spreadsheet; it’s about the health and well-being of our community, our neighbors, friends, and family members who rely on Medicaid for essential care. As an organization deeply committed to health equity, GRAAHI recognizes that any barrier to healthcare disproportionately affects our most vulnerable populations and exacerbates existing health disparities.
The Stakes Are High: What These Proposed Cuts Mean for Michigan
The proposed cuts to Medicaid, while not always direct, create significant hurdles that will make it incredibly difficult for individuals to receive and maintain their coverage. Here’s a breakdown of some key provisions and their potential impact:
- New Community Engagement Requirements (Work Requirements): These would apply to able-bodied adults aged 19-64 without dependents (with some exemptions). While presented as encouraging self-sufficiency, experience in other states shows these requirements often lead to eligible individuals losing coverage due to administrative burdens, even if they are working or exempt. It’s estimated that nearly 200,000 Michiganders could lose coverage under such requirements.
- Cost Sharing for Medicaid Expansion Enrollees: Individuals with incomes over 100% of the federal poverty level would be required to pay out-of-pocket costs. Research consistently demonstrates that even small cost-sharing amounts can act as a significant barrier to accessing necessary care, leading to reduced utilization and increased financial burden for low-income families.
- Increased Frequency of Eligibility Determination: Medicaid expansion enrollees would need to re-determine their eligibility every six months, rather than every twelve. This increased administrative burden could lead to coverage gaps for individuals who struggle to navigate complex paperwork or have fluctuating circumstances.
- Reduced Retroactive Medicaid Coverage: The retroactive coverage period would shrink from 90 days to 30 days. This is a critical change, as it means individuals who incur unexpected medical expenses before their Medicaid application is fully processed would have significantly less time for those costs to be covered, potentially leading to crippling medical debt.
- Prohibition of Medicaid and CHIP Coverage for Gender-Affirming Care for Minors: This provision directly impacts a specific and vulnerable group, denying them access to medically necessary care.
- Freezing Provider Taxes: This measure would freeze existing provider taxes and prohibit new ones. States utilize these taxes to fund Medicaid programs and draw down federal matching funds. Freezing them would create significant budget shortfalls for states, forcing them to make difficult choices between raising other taxes, cutting benefits, or reducing enrollment.
These changes are not about improving healthcare; they are about creating roadblocks that will strip vital care from those who need it most, leading to worse health outcomes and increased strain on our healthcare system and economy.
Join the Fight: Your Voice Matters!
The time to act is NOW. The campaign officially launched on Monday, May 19th, and we have a critical “Day of Action” coming up this Thursday, May 22nd, with a press event at Disability Advocates of Kent County.
GRAAHI, along with the Kent County Health Equity Council and our partners, are making it easy for every organization and every individual to participate and make their voices heard. Our collective goal is to:
- Send 15 emails: Reach out to your Members of Congress. We will provide templates and contact information to simplify this process.
- Make 15 calls: A direct phone call can be incredibly impactful. We’ll give you the tools you need to make your voice heard.
- Share social media posts from Catherine’s Health Center: Amplify the message and reach a wider audience.
- Come to the Disability Advocates event and press event on May 22nd: Stand with us in solidarity and show your support.
- Send postcards: Ask clients, patients, staff, and Board members to fill out postcards expressing their concerns. We have examples available.
- Share Your Stories: Personal stories are powerful. Collect narratives from staff and community members about how Medicaid has impacted their lives. Share these on your social media and upload them so we can share them with elected officials and the media. Anonymous submissions are welcome, but those willing to share their names can be even more impactful.
These proposed cuts threaten the health and economic stability of our community. We cannot afford to remain silent. Join GRAAHI and the Kent County Health Equity Council in this urgent campaign to protect Medicaid. Your action, no matter how small, can make a significant difference.
Together, we can safeguard access to healthcare for all Michiganders.