lupus
90% of people with lupus are women. Lupus is 2-3 times more prevalent among women of color than among Caucasian women.
LUPUS
life beyond illness
90% of people with lupus are women. Lupus is 2-3 times more prevalent among women of color than among Caucasian women.
What is lupus?
- Lupus is a chronic autoimmune disease that occurs when your body’s immune system attacks your own tissues and organs. Inflammation caused by lupus can affect many different body systems — including your joints, skin, kidneys, blood cells, brain, heart and lungs.
- Lupus is more common among women of childbearing age (ages 15 to 44 years).
symptoms
Many symptoms of lupus occur in other illnesses. Sometimes lupus is called “the great imitator” because its symptoms can be similar to symptoms of diabetes, thyroid problems, rheumatoid arthritis, blood disorders, Lyme disease, fibromyalgia, as well as many types of heart, lung, bone, and muscle diseases.
Lupus symptoms also usually come and go, meaning that you don’t have them all of the time. Lupus is a disease of flares (the symptoms worsen and you feel ill) and remissions (the symptoms improve and you feel better).
The most common symptoms of lupus (which are the same for men and women) are:
- Extreme fatigue (tiredness)
- Headaches
- Painful or swollen joints
- Fever
- Anemia (low numbers of red blood cells or hemoglobin, or low total blood volume)
- Swelling (edema) in feet, legs, hands, and/or around eyes
- Pain in chest on deep breathing (pleurisy)
- Butterfly-shaped rash across cheeks and nose
- Sun- or light-sensitivity (photosensitivity)
- Hair loss
- Abnormal blood clotting
- Fingers turning white and/or blue when cold (Raynaud’s phenomenon)
- Mouth or nose ulcers
Risk Factors
- Getting older
- Genetic mutations
- Having dense breasts.
- Personal history of breast cancer
- Family history of breast or ovarian cancer
Ways to Prevent
There is no way to prevent lupus. The cause is unknown. The only known risks are things that can’t be changed. These are things like one’s sex, age, family history, and ethnic background.
You can reduce the impact of lupus by avoiding triggers, such as:
- Sunlight. Exposure to the sun may bring on lupus skin lesions or trigger an internal response in susceptible people.
- Infections. Having an infection can initiate lupus or cause a relapse in some people.
- Medications. Lupus can be triggered by certain types of blood pressure medications, anti-seizure medications and antibiotics.
- People who have drug-induced lupus usually get better when they stop taking the medication. Rarely, symptoms may persist even after the drug is stopped.
- Be physically active
- Eat healthy meals
- Get plenty of rest
- Avoid smoking
- Wear sunscreen and avoid excessive sun exposure
Types of Lupus
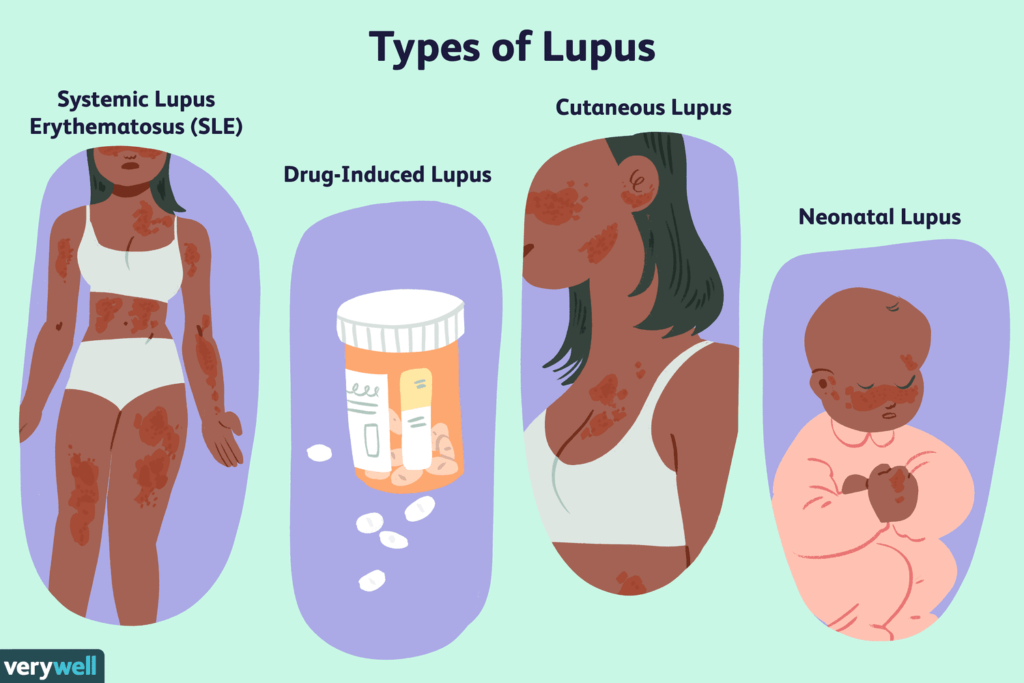
There are three main types of Lupus:
Systemic lupus erythematosus (SLE) is the most common form of lupus. A person with SLE may have mild or serious symptoms and usually affects a person between the ages of 15-45.
Cutaneous lupus erythematosus (CLE) only affects the skin. Symptoms include rashes, hair loss, swelling of the blood vessels, ulcers, and sun sensitivity.
Types of CLE include:
Chronic cutaneous (discoid) lupus- a red, raised rash may appear on the face, scalp or elsewhere. The raised areas may become thick and scaly. A small percentage of people with discoid lupus later develop SLE.
Subacute cutaneous lupus- causes skin lesions that appear on parts of the body exposed to sun.
Acute cutaneous lupus– lesions occur when your systemic lupus is active. This includes the “butterfly rash.”
Drug-induced lupus refers to a form of lupus caused by the use of certain medications. The symptoms go away when the drug is stopped.
Neonatal lupus (NL) is an autoimmune disease in which passive transfer of autoantibodies from the mother to the fetus results in fetal and neonatal disease. The major manifestations are cardiac and cutaneous findings.
treatment
Lupus is a chronic disease with no cure, thus it can only be managed. The goal of treatment is to improve symptoms, prevent flares, and prevent other health problems often caused by lupus.
Treatment for lupus depends on your signs and symptoms and requires a careful discussion of the benefits and risks with your doctor. It may include:
- Over-the-counter NSAIDs (naproxen, ibuprofen, etc.) help reduce mild pain and swelling in joints and muscles
- Antimalarial drugs to help with joint pain, skin rashes, fatigue, and lung inflammation
- Corticosteroids and Prednisone help reduce swelling, tenderness, and pain
- Immunosuppressants to help keep your immune system from attacking your body
- Biologics to help your immune system work correctly
What to do if you are at risk?
Contact your primary care physician. If you are experiencing any of the above symptoms they can help you determine if you are suffering from lupus.
Lupus can cause damage to many different parts of the body. Based on what you are experiencing you may need to see a:
- Rheumatologist- a doctor that specializes in diseases of the joints and muscles
- Immunologist- a doctor who specializes in immune system disorders
- Dermatologist- a doctor who specializes in diseases of the skin such as cutaneous lupus
- Cardiologist – a doctor who specializes in diseases of the heart
- Nephrologist – a doctor who specializes in diseases of the kidney
STATISTICS FOR PEOPLE OF COLOR
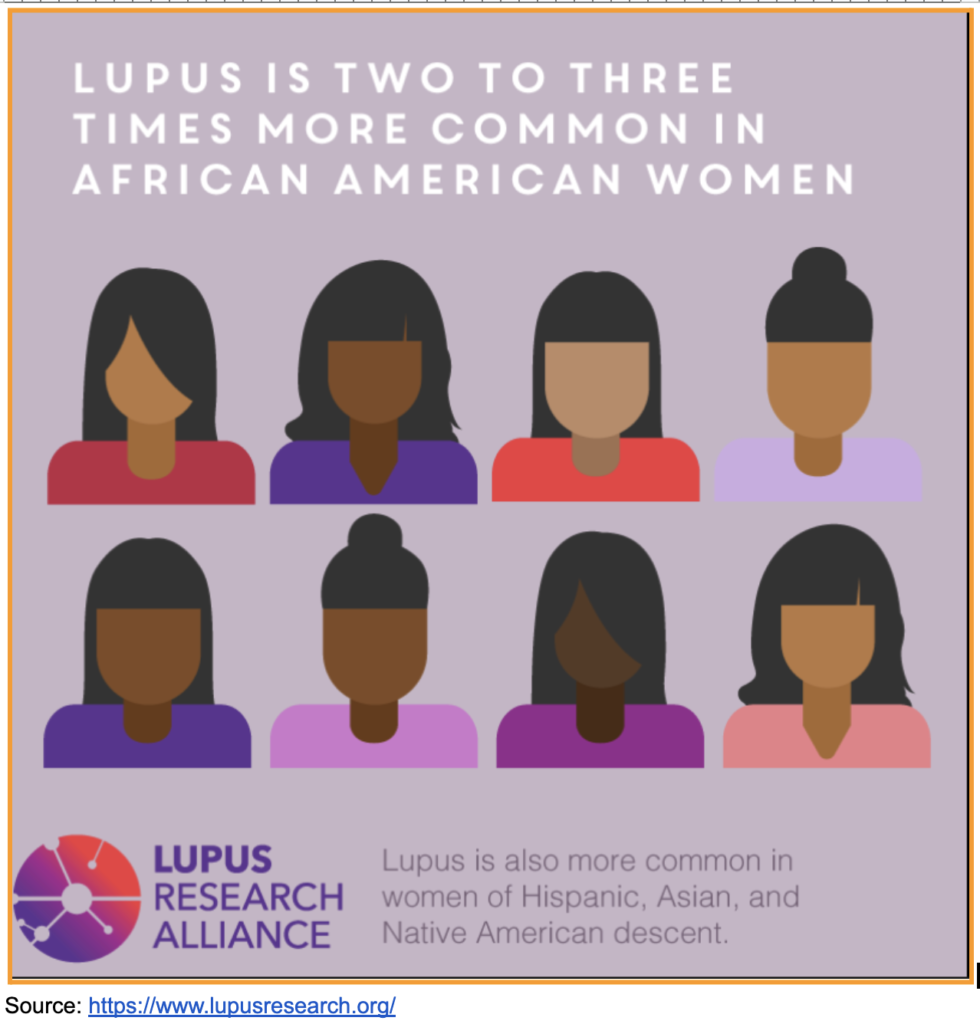
- Lupus is 2-3 times more prevalent among women of color than among Caucasian women, affecting 1 in 537 young African American women.
- African American lupus patients tend to develop lupus at a younger age, experience more serious complications, and have higher mortality rates.
- 90% of people with lupus are women

Learn more about the Stats at GRAAHI's Health Equity Index
Links, Tools, Resources
Websites
Links to resources- assessments, diagnostic tools, more specific information/subtopics
- Check if your symptoms could be related to lupus: https://www.lupus.org/resources/could-it-be-lupus
- Find support near you: https://www.lupus.org/resources/find-support-near-you
Grand Rapids/Kent County/Michigan Resources:
https://www.healthgrades.com/find-a-doctor/michigan/best-doctors-for-lupus-in-grand-rapids
https://www.uofmhealth.org/conditions-treatments/rheumatology/lupus
Latest Advances, Clinical Trials & Breakthroughs in High Blood Pressure:
https://www.webmd.com/lupus/latest-research-lupus-treatment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8972918/
https://www.lupus.org/advancing-research
https://www.lupusresearch.org/